- A-
- A+
What is Demodex?
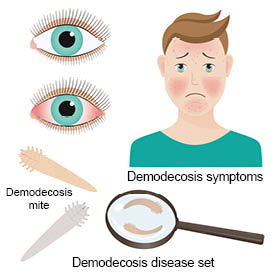 Demodex is an eight-legged mite from the Demodicidae family. There are many species of Demodex but only two of them are found present in humans, demodex folliculorum and demodex brevis.
Demodex is an eight-legged mite from the Demodicidae family. There are many species of Demodex but only two of them are found present in humans, demodex folliculorum and demodex brevis.Demodex mites are found naturally on the faces of human beings from childhood, but especially after the age of 18. Their presence on the skin increases with age.
They live in or around hair follicles (from where hair grows) and sebaceous glands (glands attached to the hair follicles that secrete sebum, an oily substance which prevents the skin and hair from drying out)1.
They form part of what is called the cutaneous microbiota or cutaneous microbial flora, in other words the micro-organisms that naturally live on our skin.
Evolution
Demodex mites need humans in order to live, they develop naturally on our skin until their death2.
The life cycle from the egg to the adult mite lasts between 14 and 18 days. The eggs are deposited in the sebaceous glands and hair follicles, they then turn into larvae until they reach adult form.
In some cases, larger numbers of Demodex develop which is thought to lead to substantial inflammation and result in the appearance of skin lesions. The mechanism behind these reactions, however, is not fully understood.
What are the symptoms of Demodex?
Demodex mites are not considered to be actual carriers of disease.
However, these parasites may generate conditions that favour the appearance of certain symptoms and pathologies in cases where larger numbers develop on the skin.
During their lifetime, they accumulate waste in their abdomens, which is only released at their death.
In cases where they become too prevalent, this release of residues can cause skin irritation and redness due to chronic inflammation and the development of vascular abnormalities3.
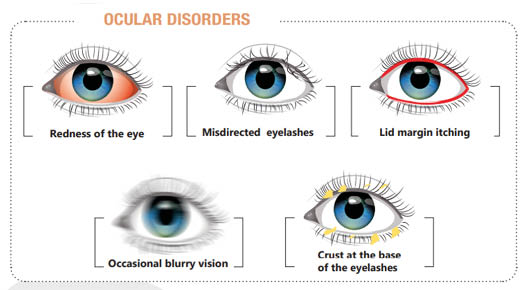
Demodex on the eyelids and blepharitis
Demodex can be the cause of Blepharitis, which is an inflammation of the edge of the eyelid4.
Demodex Blepharitis manifests itself as non-specific clinical symptoms present in all types of Blepharitis, regardless of the cause (bacteria, viruses, etc.), including:
- Redness and itching of the edge of the eyelid
- Grittiness or a foreign body sensation
- Loss of eyelashes
- In severe forms, swelling of the eyelids, painful ulcers on the eyelid edges.
It may include some signs such as:
- A pigmentation of the eyelid edge5;
- The presence of transparent or whitish flakes forming crusty debris over approximately 1 mm of the base of the lashes: this is the most characteristic and frequent sign and referred to as cylindrical dandruffs 6 7.
The diagnosis of Demodex Blepharitis is confirmed by the microscopic analysis of an eyelash sample or by visualisation of the parasites with a slit lamp (40-fold magnification) during a consultation with an ophthalmologist.
Demodex and Rosacea manifestations
Demodex also generates conditions that favour the development of Couperose or Rosacea, resulting in the dilation of small vessels under the facial skin.
Redness appears on the cheeks, the sides of the nose, the forehead and chin. As the disease progresses, the symptoms become permanent. As the disease develops, it often leads to the appearance of small red pimples (or papules).
This facial pathology generally affects adults over 20 years of age, peaking between 40 and 50 years of age8.
The severity of Rosacea is linked with ocular conditions such as Xerophtalmia (dry eye), Conjunctivitis, or even Keratitis (condition of the cornea) or Blepharitis (see above).
Evidence of excess Demodex can be shown through a skin squama analysis.
Treatment for Demodex
 After diagnosis, your ophthalmologist will recommend treating Demodex Blepharitis with a specific daily eye care routine.
After diagnosis, your ophthalmologist will recommend treating Demodex Blepharitis with a specific daily eye care routine.
As recently described in an international guideline9 the management of Demodex blepharitis requires dedicated treatments such as topical products containing tea tree oil.
The tea tree, an Australian shrub traditionally used by Aboriginal people for its medicinal properties, is known to have exceptional antiseptic properties. This natural product exhibits antimicrobial, anti-inflammatory properties and is toxic to Demodex9. More specificially terpinen 4 ol, the active and most abundant component of Tea Tree oil, that allows reducing the risk of toxicity to the ocular surface compared to non purified TTO and is an appropriate treatment for Demodex Blepharitis.11
In cases where the treatment is not successful or for more severe forms of the condition, an antibiotic or anti-parasitic treatment may be prescribed by an ophthalmologist and used in addition to a daily cleansing routine.
Treating Rosacea
Treatments for Rosacea and Couperose vary depending on the form of the condition.11
For cases of Erythmatotelangiectasic Rosacea, vascular laser treatment or a gel with an anti-glaucomatous (alpha-2 adrenergic) agent, which reduces redness thanks to its vasoconstrictive action, are used.
For cases of Papulopustular Rosacea, antibiotic or anti-parasitic treatments may be prescribed by an ophthalmologist, often in combination with a specific daily cleansing routine.
Rhinophyma, however, is treated surgically or by carbon dioxide laser.
It should be noted that the treatment of demodex is suspensive, meaning that once symptoms have subsided, recurrences are likely.
In order to avoid recurrences, the best prevention consists of an appropriate daily cleansing routine, for example, cleaning the eyelids with appropriate wipes. Sun protection is also recommended to prevent recurrence of the condition.
Artificial tears without preservatives are helpul in cases where dry eye is also an issue. Important element:dermocorticoids are contraindicated in rosacea, as they tend to aggravate lesions.3
Sources :
(1) M.-S. Thoemmes, D.-J. Fergus, J. Urban, M. Trautwein, R.-R. Dunn, “Ubiquity and Diversity of Human-Associated Demodex Mites”, 27 August 2014
https://doi.org/10.1371/journal.pone.0106265
(2) Dr S. Fauquier, “Les blépharites infectieuses : diagnostic et prise en charge”, Pratiques en ophtalomologie, février-mars 2015, no. 80
(3) Ibid.
(4) B. Kamoun, M. Fourati, J. Feki, M. Mlik, F. Karray, A. Trigui, S. Ellouze, B. Hammami, M. Chaabouni, A. Ayadi, “Blépharite à demodex : mythe ou réalité ?”, Journal français d’ophtalmologie (JFP), vol. 22, no. 5, 1999
(5) H. Sarraux, J. Blamoutier, “Les facteurs allergiques dans les blépharites chroniques”, Année thérapeutiques et cliniques en ophtalmologie, vol. XXXII, 1981
(6) S.-P. Liotet, P. Cochet, “Le demodex, son importance en contactologie”, Contactologia, 1979
(7) M. Norn, “L’acarien Demodex Folliculorum hominis, son importance en ophtalmologie”, Contactologia, 1981
(8) Dr A. Badaoui, Dr E. Mahé, “Dermatoses faciales”, La Revue du praticien, October 2018
(9) L. Jones et al. TFOS DEWS II Management and Therapy Report. The Ocular Surface 2017;583-584.
(10) Tighe S, Gao YY, Tseng SC. Terpinen-4-ol is the Most Active Ingredient of Tea
Tree Oil to Kill Demodex Mites. Transl Vis Sci Technol 2013; 2 (7): 2.
(11) Dr A. Badaoui, Dr E. Mahé, “Dermatoses faciales”, op. cit.